Endodontics
Endodontics is a field of dentistry that focuses on the dental pulp and root canal system. The dental pulp is the soft tissue inside the tooth that contains nerves, blood vessels, and connective tissue.
The root canal system is the network of nerves within the center of each tooth root.
Endodontic treatment is necessary when the dental pulp becomes inflamed or infected, which can occur due to trauma, deep decay, or other issues.
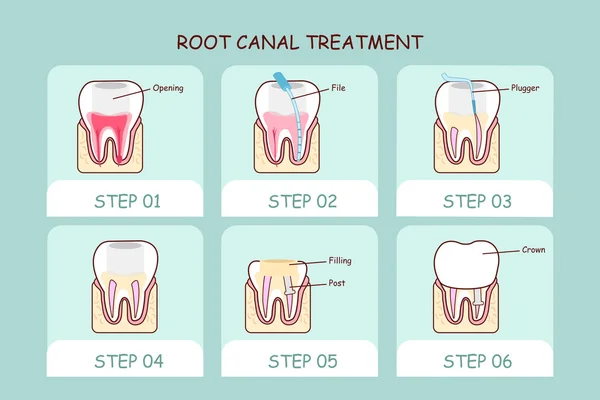
Root canal therapy is a common treatment that involves removing the damaged or infected pulp from the tooth, cleaning and shaping the root canals, and filling them with a biocompatible material to seal them and prevent further infection.
At our practice, we use the latest technology and techniques to ensure the most accurate diagnosis and effective treatment of endodontic issues. Our dentists are dedicated to providing a comfortable and stress-free experience for our patients, and will work closely with you to develop a personalized treatment plan that meets your specific needs and goals.
If you’re experiencing tooth pain or discomfort, it’s important to seek prompt treatment to prevent further damage or infection. Contact us today to schedule a consultation with one of our experienced doctors.

